We currently offer a comprehensive selection of web-based self-study courses which cover basic and advanced concepts for Passy Muir® Valve assessment and application.
In addition to self-study courses, Passy Muir also offers live continuing education through Zoom. To see our weekly schedule, and for more information, please click here.
To contact Passy-Muir or a clinical specialist with questions, please email info@passymuir.com
For ASHA: Passy Muir makes submissions to ASHA monthly, after each month has ended. Therefore, the date of completion that appears on your Continuing Education Registry is the last date of the month in which you completed the self-study course. Please refer to the CEU FAQ for more information on when courses you have taken will appear on your transcript.
For AARC: Passy Muir makes submissions to AARC every 60 days. Please refer to the CEU FAQ for more information on when courses you have taken will appear on your transcript.
Disclosure: Passy-Muir, Inc. has developed and patented a licensed technology trademarked as the Passy Muir® Tracheostomy & Ventilator Swallowing and Speaking Valve. These presentations will focus primarily on the bias-closed position Passy Muir Valve and will include little to no information on other speaking valves. Please note that Passy Muir submits both ASHA and AARC on your behalf. Because different organizations assign credit according to their own standards, we encourage you to research your organization’s requirements for Continuing Education Units. Unless otherwise stated, courses are 1 hour in length.
Getting Started Webinars
Nicole DePalma, MS, CCC-SLP
Passy Muir Clinical Consultant
Gail M. Sudderth, RRT
Passy Muir Clinical Specialist
Gail M. Sudderth, RRT
Passy Muir Clinical Specialist
Mike Harrell, BS, RRT
Director of Clinical Education-Respiratory, Passy Muir
Gail M. Sudderth, RRT
Passy Muir Clinical Specialist
Ventilator Application Webinars
Mike Harrell, BS, RRT
Director of Clinical Education-Respiratory, Passy Muir
Carrie Windhorst, MS, CCC-SLP
Cheryl Wagoner, MS, CCC-SLP
Ricque Harth, MEd, CCC-SLP
Madonna Rehabilitation Hospital, Lincoln, NE
Swallowing Webinars
Lori Burkhead-Morgan, PhD, CCC-SLP
University of Georgia, GA
Gail M. Sudderth, RRT
Passy Muir Clinical Specialist
Mary Spremulli, MA, CCC-SLP
Passy Muir Clinical Consultant
Cheryl Tansley MS, CCC-SLP
Rachel Ieronimo, MS, CCC-SLP
Gaylord Hospital, Wallingford, CT
Carmin Bartow, MS, CCC-SLP
Vanderbilt University Medical Center, Nashville, TN
Pediatric Webinars
Katy Peck, MA, CCC-SLP, CBIS
Children’s Hospital of Los Angeles, Los Angeles, CA
Katy Peck, MA, CCC-SLP, CBIS
Children’s Hospital of Los Angeles, Los Angeles, CA
Catherine S. Shaker, MS, CCC-SLP, BRS-S
Cari L. Mutnick, MA, CCC-SLP
Florida Hospital for Children, Orlando, FL
Melanie Stevens MS, CCC-SLP
Jennifer Finch, MA, CCC-SLP
Erin Wishloff, BS, RRT-NPS
Leslie Justice, RN, MS, CPN
Nationwide Children’s Hospital, Columbus, OH
Katy Peck, MA, CCC-SLP, CBIS
Children’s Hospital Los Angeles, CA
Christina Costa, MS, CCC-SLP
All Children’s Hospital, St. Petersburg, FL
Specific Diagnoses Webinars
Nicole DePalma, MS, CCC-SLP
Passy Muir Clinical Consultant
Linda Stachowiak, MS, CCC-SLP, BRS-S
MD Anderson Cancer Center, Orlando, FL
Rebecca Wills, BA, LRCP, CRT-NPS
Madonna Rehabilitation Hospital, Lincoln, NE
Leigh Anne Baker, MS, CCC-SLP, BCS-S
Promise Hospital, Baton Rouge, LA
Kelly Abry, BA, AS, CRT
Promise Hospital, Baton Rouge, LA
Special Focus Webinars
Mike Harrell, BS, RRT
Director of Clinical Education-Respiratory, Passy Muir
Randi Lynne Morgan, MA, CCC-SLP
Supervising Speech Language Pathologist at Mealtime Connections in Tucson, AZ
Heather Kuzara, RN
Creator and Director BAYADA Home Health Care Nursing Simulation Lab
Erin Ward, MS Ed, CAS
Faculty Associate Children’s Hospital Boston
Stan Perch, RRT, RPFT
Respiratory Therapist, Nurse On Call
Mary Beth Happ, PhD, RN, FAAN
The Ohio State University, Columbus, OH
Rebecca Wills, BA, LRCP, CRT-NPS
Madonna Rehabilitation Hospital, Lincoln, NE
Debra Gurnari, RRT
Kindred Hospital Wyoming Valley
Cheryl M. Martin, MS, CCC-SLP
Kindred Hospital Wyoming Valley
Overcoming Barriers to Speaking Valve Use: Success through Teamwork
Click the link above to view this course in the Passy Muir Education Portal
- If you are not logged in to the Education Portal, please do so after clicking the link
- If you do not have an Education Portal account, please create one
- You will be taken to the Course View page for this topic after logging in
Aerodigestive and Respiratory Changes Post Tracheostomy: A Comprehensive Review
Click the link above to view this course in the Passy Muir Education Portal
- If you are not logged in to the Education Portal, please do so after clicking the link
- If you do not have an Education Portal account, please create one
- You will be taken to the Course View page for this topic after logging in
Tracheostomy: Procedures, Timing and Tubes
Click the link above to view this course in the Passy Muir Education Portal
- If you are not logged in to the Education Portal, please do so after clicking the link
- If you do not have an Education Portal account, please create one
- You will be taken to the Course View page for this topic after logging in
Interdisciplinary Tracheostomy Team: Where Do I start?
Click the link above to view this course in the Passy Muir Education Portal
- If you are not logged in to the Education Portal, please do so after clicking the link
- If you do not have an Education Portal account, please create one
- You will be taken to the Course View page for this topic after logging in
Application of Passy Muir Swallowing and Speaking Valves
Click the link above to view this course in the Passy Muir Education Portal
- If you are not logged in to the Education Portal, please do so after clicking the link
- If you do not have an Education Portal account, please create one
- You will be taken to the Course View page for this topic after logging in
Passy Muir® Valve FAQ Challenge
Click the link above to view this course in the Passy Muir Education Portal
- If you are not logged in to the Education Portal, please do so after clicking the link
- If you do not have an Education Portal account, please create one
- You will be taken to the Course View page for this topic after logging in
Ventilator Basics for the Non-Respiratory Therapist*
Click the link above to view this course in the Passy Muir Education Portal
- If you are not logged in to the Education Portal, please do so after clicking the link
- If you do not have an Education Portal account, please create one
- You will be taken to the Course View page for this topic after logging in
Ventilator Application of the Passy Muir® Valves
Click the link above to view this course in the Passy Muir Education Portal
- If you are not logged in to the Education Portal, please do so after clicking the link
- If you do not have an Education Portal account, please create one
- You will be taken to the Course View page for this topic after logging in
Interdisciplinary Decision Making with Patients Requiring Tracheostomy and Mechanical Ventilation
Click the link above to view this course in the Passy Muir Education Portal
- If you are not logged in to the Education Portal, please do so after clicking the link
- If you do not have an Education Portal account, please create one
- You will be taken to the Course View page for this topic after logging in
Early SLP Intervention for the Ventilated ICU Patient: Use it or Lose It!
Click the link above to view this course in the Passy Muir Education Portal
- If you are not logged in to the Education Portal, please do so after clicking the link
- If you do not have an Education Portal account, please create one
- You will be taken to the Course View page for this topic after logging in
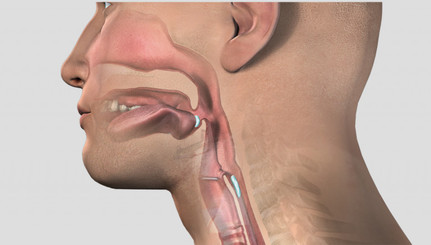
How You Breathe Matters: Swallowing Safely
Click the link above to view this course in the Passy Muir Education Portal
- If you are not logged in to the Education Portal, please do so after clicking the link
- If you do not have an Education Portal account, please create one
- You will be taken to the Course View page for this topic after logging in
Swallow Function: Passy Muir® Valve Use for Evaluation & Rehabilitation
Click the link above to view this course in the Passy Muir Education Portal
- If you are not logged in to the Education Portal, please do so after clicking the link
- If you do not have an Education Portal account, please create one
- You will be taken to the Course View page for this topic after logging in
Swallowing Management of the Tracheostomized Adult Patient – Case Studies
Click the link above to view this course in the Passy Muir Education Portal
- If you are not logged in to the Education Portal, please do so after clicking the link
- If you do not have an Education Portal account, please create one
- You will be taken to the Course View page for this topic after logging in
Pediatric Candidacy for Speaking Valve Use: Journeys to Success
Click the link above to view this course in the Passy Muir Education Portal
- If you are not logged in to the Education Portal, please do so after clicking the link
- If you do not have an Education Portal account, please create one
- You will be taken to the Course View page for this topic after logging in
Passy Muir® Valve: Keeping It On and Therapeutic Steps to Follow
Click the link above to view this course in the Passy Muir Education Portal
- If you are not logged in to the Education Portal, please do so after clicking the link
- If you do not have an Education Portal account, please create one
- You will be taken to the Course View page for this topic after logging in
Baby Trachs: Passy Muir Valve in the NICU to Optimize Swallowing and Feeding
Click the link above to view this course in the Passy Muir Education Portal
- If you are not logged in to the Education Portal, please do so after clicking the link
- If you do not have an Education Portal account, please create one
- You will be taken to the Course View page for this topic after logging in
Developing a Passy Muir Valve Protocol in the NICU
Click the link above to view this course in the Passy Muir Education Portal
- If you are not logged in to the Education Portal, please do so after clicking the link
- If you do not have an Education Portal account, please create one
- You will be taken to the Course View page for this topic after logging in
Pediatric Tracheostomy and Use of the Passy Muir® Valve
Click the link above to view this course in the Passy Muir Education Portal
- If you are not logged in to the Education Portal, please do so after clicking the link
- If you do not have an Education Portal account, please create one
- You will be taken to the Course View page for this topic after logging in
Pediatric Ventilator Application of the Passy Muir® Valve
Click the link above to view this course in the Passy Muir Education Portal
- If you are not logged in to the Education Portal, please do so after clicking the link
- If you do not have an Education Portal account, please create one
- You will be taken to the Course View page for this topic after logging in
Swallowing Management of Tracheostomized Pediatric Patient – Case Studies
Click the link above to view this course in the Passy Muir Education Portal
- If you are not logged in to the Education Portal, please do so after clicking the link
- If you do not have an Education Portal account, please create one
- You will be taken to the Course View page for this topic after logging in
Communication and Swallowing Management for ALS Patients with Tracheostomy
Click the link above to view this course in the Passy Muir Education Portal
- If you are not logged in to the Education Portal, please do so after clicking the link
- If you do not have an Education Portal account, please create one
- You will be taken to the Course View page for this topic after logging in
Passy Muir® Valve Use with the Head and Neck Cancer Population
Click the link above to view this course in the Passy Muir Education Portal
- If you are not logged in to the Education Portal, please do so after clicking the link
- If you do not have an Education Portal account, please create one
- You will be taken to the Course View page for this topic after logging in
The Role of the Passy Muir® Valve in the Pulmonary Management of the Patient with a Spinal Cord Injury
Click the link above to view this course in the Passy Muir Education Portal
- If you are not logged in to the Education Portal, please do so after clicking the link
- If you do not have an Education Portal account, please create one
- You will be taken to the Course View page for this topic after logging in
Early Intervention in Persons with Minimally Conscious State and Tracheostomy
Click the link above to view this course in the Passy Muir Education Portal
- If you are not logged in to the Education Portal, please do so after clicking the link
- If you do not have an Education Portal account, please create one
- You will be taken to the Course View page for this topic after logging in
The Home Care Trach Team: Navigating and Networking
Click the link above to view this course in the Passy Muir Education Portal
- If you are not logged in to the Education Portal, please do so after clicking the link
- If you do not have an Education Portal account, please create one
- You will be taken to the Course View page for this topic after logging in
End-of-Life Care and Patient Communication in Critical Care Settings
Click the link above to view this course in the Passy Muir Education Portal
- If you are not logged in to the Education Portal, please do so after clicking the link
- If you do not have an Education Portal account, please create one
- You will be taken to the Course View page for this topic after logging in
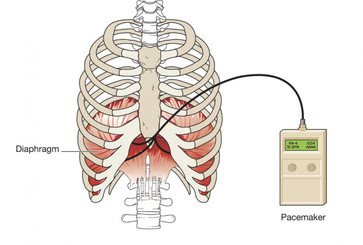
Speaking Valve and Diaphragm Pacing: Changing Lives
Click the link above to view this course in the Passy Muir Education Portal
- If you are not logged in to the Education Portal, please do so after clicking the link
- If you do not have an Education Portal account, please create one
- You will be taken to the Course View page for this topic after logging in
‘Yes You Can!’ Cardiopulmonary Rehabilitation for the Tracheostomy and Ventilator Patient
Click the link above to view this course in the Passy Muir Education Portal
- If you are not logged in to the Education Portal, please do so after clicking the link
- If you do not have an Education Portal account, please create one
- You will be taken to the Course View page for this topic after logging in
There’s More to Life than Breathing
Patients undergoing tracheostomy for long-term ventilation may face uncertainties about what their future ability to communicate will be. Clear and uninterrupted verbal communication is possible through the use of the Passy Muir® Tracheostomy & Ventilator Swallowing and Speaking Valve.
Please join Jack Rushton, a home ventilator user and Linda Dean, RRT, for an informational webinar about the use of the Passy Muir Valve. Jack will provide a first-hand account of his experience using the Passy Muir Valve, including the first time he tried it and the many ways it has enhanced his life over the 22 years he has been using it. Practical and clinical information will be provided by Linda, including successful placement of the valve in-line with the ventilator and the many clinical benefits beyond communication that the valve has to offer. Appropriate ventilator adjustments, connection options within the circuit, and transitioning and troubleshooting tips are included in this webinar.
Click the link above to view this course in the Passy Muir Education Portal
- If you are not logged in to the Education Portal, please do so after clicking the link
- If you do not have an Education Portal account, please create one
- You will be taken to the Course View page for this topic after logging in

All self-study webinars are .1 ASHA CEUs (Intermediate level; Professional area) unless otherwise noted on the webinar itself.

Passy-Muir, Inc. is an approved provider of continuing education by the Continuing Respiratory Care Education (CRCE) system of the American Association of Respiratory Care (AARC).

Passy-Muir, Inc. is an approved provider of continuing education by the California Board of Registered Nursing (Provider #CEP112390).

Nicole received her Bachelors Degree at Georgetown University and subsequently earned her Masters at New York Medical College in Speech Language Pathology.
Nicole previously worked as the Director of Speech-Language Pathology at Barlow Respiratory Hospital and Research Center, a long-term acute care facility that specializes in medically complex populations including tracheostomy and ventilator-dependent patients.
She was instrumental in developing and implementing new protocols, performance improvement strategies, and providing comprehensive education to clinical staff.
Through her leadership, the Passy Muir® Valve was made a standard of practice for all patients, including those on mechanical ventilation. In addition, she has experience in acute, sub-acute and skilled nursing facility settings.
Disclosure:
Financial –
Nicole DePalma was employed by Passy Muir and received a salary at the time the course was recorded.
Nonfinancial –
No relevant nonfinancial relationship exists

Linda K. Dean, RRT has 23 years of experience in acute, sub-acute, and long term care. She worked as both a clinical educator and educational consultant for Passy Muir. Her extensive knowledge of respiratory mechanics, as well as her remarkable teaching skills, makes her an extremely effective instructor. She has over 20 years of experience lecturing both domestically and internationally on the areas of respiratory function, team building, and use of the Passy Muir Valve in-line with mechanical ventilation for both pediatrics and adults.
Disclosure:
Financial –
Was employed by Passy-Muir, Inc at the time of these recordings.
Nonfinancial –
No relevant nonfinancial relationship exists

Gail M. Sudderth, RRT has extensive experience in a variety of settings as a respiratory therapist. As lead therapist of a 32 bed intermediate care unit in a large teaching hospital, she was an integral member of the weaning team, and focused on the “hard to wean patient.”
A recognized speaker, she has presented at state and national medical professional meetings in the United States and Canada on the topic of airway and ventilator management and the application of the Passy Muir® Valve.
She is currently a full-time clinical specialist for Passy-Muir, Inc., while continuing her clinical practice as a per diem staff therapist in northern Virginia.
Disclosure:
Financial –
Employee of Passy-Muir, Inc.
Nonfinancial –
No relevant nonfinancial relationship exists

Julie Kobak, MA, CCC-SLP received her B.S. and M.A. at Kent State University in Kent, Ohio. She has been a certified and licensed speech language pathologist for 19 years and was formerly employed as Vice President of Clinical Education at Passy-Muir, Inc.
She has worked with tracheostomized and ventilator-dependent patients at both pediatric and adult rehabilitation hospitals, including the Cleveland Clinic Children’s Hospital for Rehabilitation.
As a clinical educator, she has provided numerous lectures and inservices on the topic of tracheostomy and Passy Muir® Speaking Valves at hospitals and conferences nationally and internatinally.
Julie has also worked as a clinical supervisor and educational supervisory liaison at Kent State University.
Disclosure:
Financial –
Julie Kobak was employed by Passy Muir and received a salary at the time the course was recorded.
Nonfinancial –
No relevant nonfinancial relationship exists

Mike Harrell, BS, RRT was formerly Director of Respiratory Care with Charlotte Regional Medical Center (CRMC) in Punta Gorda, FL for several years prior to joining the Passy Muir Educational Team as a Passy Muir Clinical Specialist in 2005.
Mike presided as president of the Florida Society of Respiratory Care where he brought his clinical knowledge and strong advocacy for patient care together to improve respiratory care in the state of Florida.
His CRMC team’s clinical work with trach and vent was highlighted in the Joint Commission Perspective on Patient Safety, February 2003 issue, which discussed implementing a performance improvement team to implement the written policies and procedures for tracheostomized patients.
This critical pathway put into action the use of the Passy Muir® Valves for ventilator-dependent patients after early consideration of tracheostomy for the patient. This policy resulted in faster weaning from the ventilator, less time in the ICU and fewer readmissions at CRMC.
Disclosure:
Financial –
Employee of Passy-Muir, Inc.
Nonfinancial –
No relevant nonfinancial relationship exists

Carrie Windhorst, MS, CCC-SLP is employed with Madonna Rehabilitation Hospital. Her primary caseload is served on the Long Term Acute Care Hospital (LTACH) Unit which focuses on tracheostomy and ventilator weaning.
She serves as a consult therapist in the acute care setting at The Nebraska Heart Hospital and provides guest lectures at the University of Nebraska-Lincoln.
Disclosure:
Financial –
Financial – Received a speaking fee from Passy-Muir, Inc. for this presentation
Nonfinancial –
No relevant nonfinancial relationship exists

Cheryl Wagoner, MS, CCC-SLP is employed with Madonna Rehabilitation Hospital. She has worked on the Long Term Acute Care Hospital (LTACH) unit for the past 10.5 years providing evaluation and treatment for patients with a variety of neurological and pulmonary diagnoses and patient with tracheostomy tubes and mechanical ventilation. She also serves as a consult therapist in the acute care setting at The Nebraska Heart Hospital and provides guest lectures at the University of Nebraska-Lincoln.
Disclosure:
Financial –
Received a speaking fee from Passy-Muir, Inc. for this presentation
Nonfinancial –
No relevant nonfinancial relationship exists

Ricque Harth, MEd, CCC-SLP is employed with Madonna Rehabilitation Hospital. She has worked as the lead therapist on the Spinal Cord Injury team and has worked on the Long Term Acute Care Hospital unit for the past year providing evaluation and treatment for patients with tracheostomy tubes and mechanical ventilation.
Disclosure:
Financial –
Received a speaking fee from Passy-Muir, Inc. for this presentation
Nonfinancial –
No relevant nonfinancial relationship exists

Dr. Burkhead Morgan has practiced speech-language pathology since 1994 in a variety of settings. She earned a PhD from the University of Florida in 2005, focusing on using exercise-based principles in dysphagia diagnosis and management.
She has presented domestically and internationally, published peer-reviewed articles and a book chapter relating to dysphagia. Her current research focuses on developing more effective approaches for dysphagia evaluation and treatment using principles of exercise science.
Disclosure:
Financial –
Received a speaking fee from Passy-Muir, Inc. for this presentation
Nonfinancial –
No relevant nonfinancial relationship exists

Mary Spremulli MA, CCC-SLP is a medical Speech-Language Pathologist with over 25 years experience. She is the Founder and President of Voice Aerobics, LLC, through which she provides therapy services to adults with speech, voice and swallowing disorders and conducts training seminars and lectures related to the care of tracheostomy patients throughout the United States and Puerto Rico.
Ms. Spremulli helped to develop a collaborative standard of care for the tracheostomized patient that received Joint Commission recognition as a model for improving patient safety and outcomes.
Disclosure:
Financial –
Received a speaking fee from Passy-Muir, Inc. for this presentation
Nonfinancial –
No relevant nonfinancial relationship exists

Cheryl Tansley, MS, CCC-SLP received her BS and MS at Worchester State College, MA and has 9 years experience as a speech pathologist in school-based and outpatient settings and as the lead speech pathologist in an acute care setting.
Currently she works at Gaylord Hospital in Wallingford, CT, a long term acute care rehabilitation hospital specializing in the medically complex population.
Cheryl is a key member of the tracheostomy and ventilator team at Gaylord Hospital and has been instrumental in the success of the program for improving patient outcomes for swallowing and decannulation.
Disclosure:
Financial –
Received a speaking fee from Passy-Muir, Inc. for this presentation
Nonfinancial –
No relevant nonfinancial relationship exists

Rachel Ieronimo, MS, CCC-SLP received her BS degree at the University of Connecticut and her MS degree at Southern Connecticut State University.
She recently completed her clinical fellowship year at Gaylord Hospital working with the medically complex population. She has treated tracheostomized and ventilator-dependent patients, including management of dysphagia.
Disclosure:
Financial –
Received a speaking fee from Passy-Muir, Inc. for this presentation
Nonfinancial –
No relevant nonfinancial relationship exists

Carmin Bartow, MS, CCC-SLP is a speech pathologist specializing in treatment of tracheostomized and ventilator-dependent patients. She currently works at Vanderbilt University Medical Center in adult acute care and the out-patient dysphagia center.
She has gained experience in a variety of settings including ICU’s, a progressive respiratory care unit, home health, out-patient and an LTAC vent weaning facility. She is also an educational consultant for Passy-Muir, Inc.
She has presented numerous seminars and courses on communication and swallowing intervention with the tracheostomized population at local, regional, state and national conferences. She has also authored an ASHA publication entitled “Tracheostomy Tubes in Adults; Management of Communication and Swallowing Impairments”.
Disclosure:
Financial –
Received a speaking fee from Passy-Muir, Inc. for this presentation
Nonfinancial –
No relevant nonfinancial relationship exists

Katy Peck, M.A., CCC-SLP, CBIS is a Pediatric Speech-Language Pathologist with over 10 years experience with infants through young adults with complex medical needs. She is recognized as a Certified Brain Injury Specialist by the American Brain Injury Association and is ASHA board certified.
She has worked full-time at Children’s Hospital Los Angeles (CHLA) for the past 4 years, specializing in feeding/swallowing, acquired brain injury, and meeting the needs of medically fragile children who require mechanical ventilation.
She is the lead Speech Pathologist responsible for training staff in swallowing, Modified Barium Swallow Study, and assessment/treatment for patients with tracheostomy. She is the co-chair of the Dysphagia Team and active participant in the NICU Task Force developed to define the role of speech therapy in the NICU at CHLA.
She is a co-investigator for a research study designed in collaboration with the CHLA Pulmonology Department to determine safety, comfort, and overall benefits of Passy Muir® Valve use in the chronically ventilated pediatric population. This study is currently in the pre-submission stage of publication.
Disclosure:
Financial –
Received a speaking fee from Passy-Muir, Inc. for this presentation
Nonfinancial –
No relevant nonfinancial relationship exists

Christina Costa, MS, CCC-SLP received her B.A. at Asbury University in Wilmore, Kentucky and her M.S. at The University of South Florida in Tampa, Florida. She has been a certified and licensed speech language pathologist for 4 1/2 years and is currently working as an Acute Care Speech-Language Pathologist at All Children’s Hospital in Saint Petersburg, Florida.
She works with tracheostomized and ventilator-dependent patients in the NICU, pediatric population, and outpatient ventilator clinic.
She has co-taught inservices and lectures on the topics of Evaluation and Rehabilitation of Children with a Tracheostomy, and Feeding in the CVICU. Prior to becoming a Speech-Language Pathologist, she taught English as a second language for 18 years.
Disclosure:
Financial –
Received a speaking fee from Passy-Muir, Inc. for this presentation
Nonfinancial –
No relevant nonfinancial relationship exists

Catherine S. Shaker, MS/CCC-SLP, BRS-S is a Pediatric Speech-Language Pathologist at the Walt Disney Pavilion at Florida Hospital for Children, Orlando FL.
With 35 years experience in pediatrics, she is nationally recognized as an expert in and invited lecturer regarding swallowing/feeding across the continuum of pediatric settings, including neonates, medically-fragile infants, and children through school age.
An ASHA Board Recognized Specialist in Swallowing and Swallowing Disorders, Ms. Shaker has been an integral part of large Level III Neonatal Intensive Care Units for over 25 years and is known for her work on Cue-Based Feeding Approaches in the NICU.
She has published several manuscripts on NICU intervention, and co-authored The Early Feeding Skills Assessment Tool for NICU Infants.
Disclosure:
Financial –
Received a speaking fee from Passy-Muir, Inc. for this presentation
Nonfinancial –
No relevant nonfinancial relationship exists

Cari L. Mutnick, MA/CCC-SLP received her Master’s Degree at New York University in New York, New York. She has been a certified and licensed speech-language pathologist for 6 years and is currently working as an Acute Care Speech-Language
Pathologist at The Walt Disney Pavilion at Florida Hospital for Children. She works with tracheostomized and ventilator-dependent patients in the NICU and pediatric population.
Cari has co-taught in-services on the topics of the use of in-line Passy-Muir
Valves in the acute care setting and developed an NICU/pediatric protocol for use of the Passy-Muir Valve. Facility: Florida Hospital for Children – Orlando, FL
Disclosure:
Financial –
Received a speaking fee from Passy-Muir, Inc. for this presentation
Nonfinancial –
No relevant nonfinancial relationship exists

Melanie Stevens, MS, CCC-SLP has been a pediatric speech language pathologist at Nationwide Children’s Hospital in Columbus, Ohio for the past 12 years. For the last 3 years she has worked in the NICU with a primary focus on meeting the communication needs of patients with tracheostomy tubes.
Disclosure:
Financial –
Received a speaking fee from Passy-Muir, Inc. for this presentation
Nonfinancial –
No relevant nonfinancial relationship exists

Jennifer Finch, MA, CCC-SLP has been a certified and licensed pediatric speech language pathologist for 14 years and is currently working at Nationwide Children’s Hospital, Columbus, OH. She has a special interest in language/speech development of children with tracheostomies.
Disclosure:
Financial –
Received a speaking fee from Passy-Muir, Inc. for this presentation
Nonfinancial –
No relevant nonfinancial relationship exists

Disclosure:
Financial –
Received a speaking fee from Passy-Muir, Inc. for this presentation
Nonfinancial –
No relevant nonfinancial relationship exists

Jennifer Finch, MA, CCC-SLP has been a certified and licensed pediatric speech language pathologist for 14 years and is currently working at Nationwide Children’s Hospital, Columbus, OH. She has a special interest in language/speech development of children with tracheostomies.
Disclosure:
Financial –
Received a speaking fee from Passy-Muir, Inc. for this presentation
Nonfinancial –
No relevant nonfinancial relationship exists

Linda Stachowiak, MS, CCC-SLP, BRS-S is a Speech Pathologist at the MD Anderson Cancer Center, Orlando, Florida and adjunct instructor at the University of South Florida and the University of Central Florida. She is also a CAA site visitor for ASHA and frequent presenter at local, state and national conferences.
Linda has extensive clinical experience in dysphagia and head and neck cancer and tracheostomized and ventilator-dependent patients. She also participates in multi-institutional research which investigates functional outcomes in the areas of speech and swallowing with head and neck cancer patients. She is a Board Recognized Specialist in Swallowing and Swallowing Disorders.
Disclosure:
Financial –
Received a speaking fee from Passy-Muir, Inc. for this presentation
Nonfinancial –
No relevant nonfinancial relationship exists

Rebecca Wills, BA, LRCP, CRT-NPS has been on staff at Madonna Rehabilitation Hospital since 1996. As Pulmonary Program Manager, Rebecca is responsible for the development, growth, quality and marketing of programs for adult and pediatric trach and ventilator patients. Rebecca has presented on a variety of pulmonary related topics to health care professionals on a local, regional and national level.
Disclosure:
Financial –
Received a speaking fee from Passy-Muir, Inc. for this presentation
Nonfinancial –
No relevant nonfinancial relationship exists

Leigh Anne Baker, MS, CCC-SLP, is a speech-language pathologist in Baton Rouge, Louisiana. She is a 2005 graduate of Purdue University and has over 7 years of experience working with tracheostomy patients and over three years of specialized training working with patients who have tracheostomy tubes requiring mechanical ventilation in the LTAC setting.
She has presented on the local, university and state levels on communication and swallowing evaluation and treatment of patients with tracheostomy tubes requiring mechanical ventilation.
Leigh Anne is a candidate for recognition by the Specialty Board for Swallowing and Swallowing Disorders. She is also a Clinical Supervisor for Louisiana State University.
Disclosure:
Financial –
Received a speaking fee from Passy-Muir, Inc. for this presentation and is a Passy Muir Consultant.
Nonfinancial –
No relevant nonfinancial relationship exists

Mary Beth Happ, PhD, RN, FAAN is the Distinguished Professor of Critical Care Research and Director of the Center of Excellence in Critical and Complex Care at The Ohio State University College of Nursing. Previously a faculty member in the University of Pittsburgh School of Nursing for 12 years, Dr. Happ held the UPMC Health System Chair in Nursing Science with secondary appointments in Critical Care Medicine, Clinical and Translational Science and Bioethics and Health Law.
She currently holds Adjunct faculty appointments to the University of Pennsylvania and the University of Pittsburgh Schools of Nursing and Medicine, Department of Critical Care Medicine.
Her program of research is targeted to seriously ill older adults and is focused on developing and testing interventions to improve care and communication with mechanically ventilated and communication-impaired patients, symptom communication, and end-of-life care in the intensive care unit.
She has experience in testing electronic communication devices in the ICU setting using a mixed methods approach to usability and feasibility testing.
Dr. Happ led an interdisciplinary team to develop and test a multi-component intervention (nurse training, communication tools, speech-language consultation) to improve patient communication during mechanical ventilation (SPEACS). She co-led the Robert Wood Johnson Foundation INQRI project, SPEACS-2: Improving Patient Communication and Quality Outcomes in the ICU. Dr. Happ is a Fellow in the American Academy of Nursing and member of the Expert Panel on Critical Care.
She serves on the editorial boards of Heart and Lung and the Journal of Gerontological Nursing, and has authored/co-authored over 100 published articles, editorials, book chapters and educational modules.
Disclosure:
Financial –
Has published numerous book chapters, for some of which she receives royalty payments from the publishers SAGE Publications and Springer Publications Co. Received a speaking fee from Passy-Muir, Inc. for this presentation. Information for this program made possible through research funded by the Robert Wood Johnson Foundation INQRI program and the Greenwall Foundation Kornfeld Program on Bioethics and Patient Care. She is employed by The Ohio State University College of Nursing and receives a salary.
Nonfinancial –
No relevant nonfinancial relationship exists

Jack Rushton, Passy Muir® Valve User was a grandfather, author, public speaker, and full-time ventilator user. In the years since the accident that left him paralyzed from the neck down, he continued to give motivational speeches to audiences of all ages.
Disclosure:
Financial –
Received a speaking fee from Passy-Muir, Inc. for this presentation
Nonfinancial –
As a patient, utilizes the Passy Muir® Valve

Randi Lynne Morgan, MA, CCC-SLP received a Bachelors degree in Speech Language Pathology from Northern Arizona University, and a Masters degree in Speech Language Pathology from the University of Iowa.
She is the Supervising Speech Language Pathologist at Mealtime Connections in Tucson, AZ, and an Associate Clinical Professor for The University of Arizona. Randi is a speech language pathologist who has specialized in pediatric feeding and dysphagia for the past 11 years.
She has significant experience evaluating and treating premature infants, medically complex infants, toddlers, and children and developmentally delayed infants, toddlers, and children in hospital, clinic, and home settings.
Disclosure:
Financial –
No relevant financial relationship exists
Nonfinancial –
No relevant nonfinancial relationship exists

Heather Kuzara, RN began her career as a nurse in 2003 working in an adult and pediatric medical surgical unit and pediatric cardiothoracic ICU setting in Michigan.
She moved to North Carolina in 2005 and began working at BAYADA Home Health Care as a field nurse. There, she worked with a large variety of pediatric and adult tracheostomy and ventilator clients.
Through the years, she has worked as a clinical manager, office director, and most recently, creator and director of the BAYADA Home Health Care nursing simulation lab in Charlotte, NC. As the director of the simulation lab, Heather provides tracheostomy and ventilator education in a simulated home care setting with high fidelity simulator mannequins.
Heather became a Certified Senior Advisor in 2011 and is a Certified Clinical Simulation Instructor. Heather lives in Charlotte, NC with her husband Tim and two daughters, Ella and Mena. Heather has a passion for long distance running and is currently training for her third marathon.
Disclosure:
Financial –
Full-time employee at BAYADA Home Health Care
Nonfinancial –
Creator and Director of BAYADA Home Health Care Nursing Simulation Lab

Erin Ward, MS Ed, CAS, holds a Master’s Degree in Education and a Certificate of Advanced Study in Counseling and is committed to combining her personal experiences as a mother of a child with complex medical needs with her professional skills to work towards improving parent-professional relationships and the quality of healthcare for children and adults with tracheostomies.
Erin is a founding member of TrachCare, Inc., a Massachusetts-based, non-profit organization established in 2005 providing support and information to parents, caregivers, and healthcare providers of children who have, or previously had a tracheostomy (www.trachcare.org).
As a Faculty Associate for the Institute for Professionalism and Ethical Practice at Children’s Hospital Boston since 2005, Erin contributes to developing curricula and facilitates medical education programs that focus on enhancing relational and communication skills.
Erin served as the 2013 Conference Director for her son’s diagnosis community’s biennial conference, MTM-CNM Family Conference (www.mtm-cnm.com). She is also on the Board of Directors for the developing Global Tracheostomy Collaborative (www.globaltrach.org).
Disclosure:
Financial –
No relevant financial relationship exists
Nonfinancial –
Co-founder/VP TrachCare, Inc.; Board of Directors, Global Tracheostomy Collaborative
Stan Perch, RRT, RPFT, is a Registered Respiratory Therapist with 33 years of experience. He is currently employed by Nurse On Call, a home health agency in Florida since 2011. He is responsible for patient and staff education, including tracheostomy care. Through the years, he has also worked as a owner, general manager, equipment specialist, and staff supervisor.
Disclosure:
Financial –
No relevant financial relationship exists
Nonfinancial –
No relevant nonfinancial relationship exists

Debra M. Gurnari, RRT, has over 30 years of clinical experience as a respiratory care practitioner. Since 2002 she has been the the Respiratory Therapy Department Manager at Kindred Hospital Wyoming Valley in Pennsylvani where her focus is weaning and rehabilitation of adult tracheostomized and ventilator-dependent patients.
Ms. Gurnari shares her knowledge of Passy Muir valves with staff and patients to promote use and ventilator weaning. She is on the board of Kindred Healthcare, Inc. National Respiratory Council.
Disclosure:
Financial –
Received a speaking fee from Passy-Muir, Inc. for this presentation
Nonfinancial –
No relevant nonfinancial relationship exists

Cheryl M. Martin, MS, CCC-SLP has over 20 years experience as a speech-language pathologist. She currently works for RehabCare as the Director of Rehabilitation at Kindred Hospital Wyoming Valley in Wilkes-Barre, Pennsylvania where she focuses on pulmonary rehabilitation. In conjunction with the respiratory department, she has worked to promote weaning of tracheostomized and ventilator-dependent patients through movement and the use of Passy Muir Valves.
Ms. Martin has been a speaker at the annual Spring Pulmonary Seminar educating professionals about speaking valve use and its clinical benefits. As a director coach for RehabCare, she trains new directors and speech pathologists. She is a member of the American Speech and Hearing Association and is on the Rehab Leadership Advocacy Council.
Disclosure:
Financial –
Received a speaking fee from Passy-Muir, Inc. for this presentation
Nonfinancial –
No relevant nonfinancial relationship exists
Disclosure:
Financial –
Received a speaking fee from Passy-Muir, Inc. for this presentation
Nonfinancial –
No relevant nonfinancial relationship exists